Is it really possible to be metabolically healthy if you are overweight, or obese, without a lot of muscle?
Yes. I am sure it is possible, but it is not very likely and the degree to which it is possible all depends on your criteria for what is metabolically healthy. It wouldn’t be a bet I would make personally, but even if someone is overweight or obese and metabolically unhealthy, it looks like being in a caloric deficit and/or high amounts of physical activity may allow someone to become transiently metabolically healthy for 24 to 48 hours.
This probably sounds very complicated so let’s dig in.
First, even individuals who are classified as metabolically healthy obese (MHO) carry 4 times the risk of type II diabetes compared to healthy, normal-weight adults with relatively short follow-up periods [1].
MHO is also related to an increased risk of cardiovascular disease, non-alcoholic fatty liver, and cancer [2-6]. However, we do not have much long-term research on the potential effect of interventions that are able to arrest someone in an MHO phenotype and thus potentially decrease chronic disease risk over time. Given the current data available, it is likely there will still be some intermediate-level residual risk.
Furthermore, if someone is overweight or obese it might be possible, with intense physical activity and lower carbohydrate dietary interventions, to become transiently metabolically healthy [7-10]. However, it bears mentioning that without significant body composition changes these metabolic benefits are unlikely to last longer than 24-48 hours [11].
So, if it is NOT very likely that someone can be metabolically healthy at any size, one might be wondering what the likelihood of being metabolically healthy is at their current size?
This all depends on how you objectively define what it means to metabolically health.
For example, the analysis that was just published by Zhou et al., of the UK Biobank data [12] has been getting a lot of press of late. I am personally not a fan of the study design, but it is interesting that even with their extremely lax objective criteria for metabolic health that they still picked up some absolutely mind-boggling hazard ratios for the progression to type 2 diabetes in an average of just 4.4 years of follow-up (with a kitchen sink of covariates because they had the sample size to include these in their model).
They found that someone on average had:
· a 432% increased risk of progression to type 2 diabetes if they were in the metabolically healthy obese phenotype;
· a 515% increased risk of progression to type 2 diabetes if they were in the metabolically unhealthy normal-weight category;
· and a 1,286% increased risk among those categorized as metabolically unhealthy and obese.
Here is the rub…below are their classification criteria for being "metabolically healthy":
1. Fasting triglycerides less than 203 mg/dL
2. C Reactive Protein < 3 mg/dL
3. LDL cholesterol less than 116 mg/dL (and no cholesterol lowering meds)
4. HDL cholesterol greater than 39 mg/dL
5. Hemoglobin A1c < 6.0
6. Systolic Blood Pressure <130 and Diastolic Blood Pressure < 80 mmHg (and no antihypertensive meds)
“Participants who fulfilled at least four (out of six) metabolically healthy criteria were considered metabolically healthy.” [12]
WHAT!? 4 out of 6!?
If you were normal weight per a BMI classification you had a 78% shot of meeting 4 out of 6 of these criteria.
If you were obese, you had a 37% chance.
The thing is this criteria for being metabolic healthy is ridiculous and ultimately misleading.
One could easily be prediabetic and hyperlipidemic and still be considered “healthy”. Theoretically, someone could even be diabetic and hypertensive and meet their criteria for metabolic health!
Conversely, Araujo and colleagues [13] recently looked at the prevalence of metabolic health in the United States with a much stricter criteria. However, even these researchers set the criteria for metabolic health as just not being diagnosable with prediabetes. In this analysis, regardless of BMI they found that only 12.2% of Americans would be classified as having optimal metabolic health. According to their summary statement: “Prevalence of optimal metabolic health is remarkably low among U.S. adults, with one in eight Americans achieving optimal levels of the five traditional cardiometabolic risk factors without medication.”
In comparison, Dr. Tommy Wood an M.D. Ph.D. and researcher at the University of Washington and I reanalyzed NHANES data with a slightly stricter blood glucose control criteria* and a waist to height ratio of less than 0.5 and we found that only 8.6% of US Adults would be classified as metabolically healthy.
We further stratified these results by BMI category and sex*.
If a male is in the normal weight category, his likelihood of being metabolically healthy looks to be around ~20%. If he is in the overweight category, it drops to ~8.2%. If he is obese that number drops to just ~2.8%.
Females do fair better inside the current BMI breakdowns and below are the numbers:
If a female is in the normal weight category, her likelihood of being metabolically healthy looks to be around ~29.5%. If she is in the overweight category, it drops to ~15.1%. If she is obese that number drops to just ~7.3%.
The criteria we used for being categorized as metabolically healthy was: systolic blood pressure <120mmHg and diastolic blood pressure <80 mmHg; fasting glucose <100 mg/dL and hemoglobin A1c <5.5%; triglyceride <150 mg/dL, and a triglyceride to HDL ratio <2. We did not have medication data so these percentages are honestly even slightly lower. :(
I had two major takeaways from looking at all of these numbers.
1) The modern world is in dire trouble. We are 10-20 years out from possibly the most massive public health onslaught ever witnessed by our species.
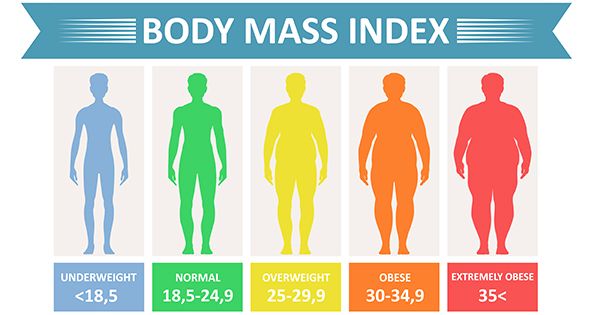
2) From this analysis it also becomes evident that BMI really isn’t that great of a predictor of metabolic health given the prevalence of central adiposity (>91%), low physical capacity, and lower muscle mass in industrialized western populations. We have to remember that BMI does no delineate between muscle, bone, and fat, and it also does not delineate between where that fat is stored. This doesn’t mean that BMI is completely without utility (although I don't really find it very useful and it has an extremely questionable origin story), but ironically what this data signals to me is the exact opposite of what many in the Anti-Diet world are trying to say about BMI.
Yes, BMI isn't highly predictive of objective health because it is actually too lax and unspecific and does not contain a measurement of body composition or fat distribution.
Furthermore, just because someone is categorized within an obese BMI doesn’t mean they are automatically unhealthy, although the odds are not very good. Perhaps, more importantly, a normal BMI within our current industrialized population absolutely does NOT guarantee metabolic health!!!
Thus, if someone doesn’t lift and exercise significantly and would be whole-heartedly classified as a modern industrial human they have about a ~20-30% shot of being objectively metabolically healthy even inside of the normal weight category and if you move into the obese category that likelihood goes down significantly.
Additionally, these studies have such low sample sizes of people who lift and maintain lower levels of body fat and thus they literally tell us NOTHING about this type of human’s risk profile. Furthermore, these lax criteria like those utilized in the Zhou et al. study above put the “health” of the normal referent population for the majority of these observational prospective trials into extreme question.
BUT, all of these analyses also begin to start a different discussion about what it means to objectively be metabolically healthy. These numbers and metrics can then potentially be utilized as points when someone would no longer be dieting or losing fat for health purposes.
There is no judgment for people wanting to lose body fat strictly because of aesthetic wants, but many times, we conflate the two. Unfortunately, many people believe they can’t be healthy without a resting 8 pack which is just not true, and in fact, the person you see on the gram with a resting 8 pack may not be that healthy anyways (covered HERE).
So let’s provide some better body composition metrics for health other than influencer aesthetics and BMI categorizations that potentially lack a large amount of predictive capacity!
· For a male to have a high likelihood of being metabolically healthy we recommend they maintain a fat-free mass index (FFMI)** of over 19, a body fat percentage under 20% [14], and a waist to height ratio of less than 0.5.
· For females, we recommend maintaining an FFMI over 16, a body fat percentage under 34% [14], and waist to height ratio of less than 0.5.
If someone meets these combined fat-free mass, body fat, and central adiposity metrics as predictors of metabolic health instead of BMI they likely triple their likelihood of being metabolically healthy.
Unfortunately, only 4.3% of men within the NHANES data set met those criteria, and just 2.6% of females which reiterates the fact that the western world is in objectively bad shape.
TL; DR - Can you be metabolically healthy and obese?
The purely scientific answer to that question looks to be yes, but the amount of individuals who fit these criteria all depends on how you define metabolically healthy. Regardless of the definition we choose, once someone fills up their subcutaneous adipose tissue stores, and starts storing fat viscerally and ectopically around their organs, they are likely going to significantly and objectively reduce their objective health [15-17]. Luckily, when we lose body fat through diet and exercise, visceral and ectopic fat look to be the first to go.
Thus, if someone has exceeded their personal fat threshold, then decreasing body fat and increasing muscle through diet and exercise is the primary way to change baseline metabolic health...and this looks to be of critical importance to a large portion of our population [18]. However, without weight loss, it is likely possible to become transiently metabolically healthy with high levels of physical activity and eating a more whole-food, nutrient-dense diet. If we focus on these big-play processes, the majority of Americans will likely lose weight (and visceral adiposity) and even maintaining a 5% weight loss will very likely increase one’s metabolic health and may reduce the risk of progression to type 2 diabetes by 89% [19].
Furthermore, even if someone focuses on getting in more activity and eating more whole foods and they don’t lose weight, they will still likely change the way their fat is distributed in a healthy way [20-22].
*We took out the waist to height ratio component when looking at the data by sex and BMI category as this is redundant.
**If you are unfamiliar with the term Fat-Free Mass Index, similar to the idea of BMI, it is an equation that quantifies the amount of muscle you have for your height. If you have even a rough idea of your body fat percentage you can calculate your FFMI here.
REFERENCES:
1. Bell, J.A., M. Kivimaki, and M. Hamer, Metabolically healthy obesity and risk of incident type 2 diabetes: a meta-analysis of prospective cohort studies. Obes Rev, 2014. 15(6): p. 504-15.
2. Chang, Y., et al., Metabolically Healthy Obesity and the Development of Nonalcoholic Fatty Liver Disease. Am J Gastroenterol, 2016. 111(8): p. 1133-40.
3. Eckel, N., et al., Transition from metabolic healthy to unhealthy phenotypes and association with cardiovascular disease risk across BMI categories in 90 257 women (the Nurses' Health Study): 30 year follow-up from a prospective cohort study. Lancet Diabetes Endocrinol, 2018. 6(9): p. 714-724.
4. Eckel, N., et al., Metabolically healthy obesity and cardiovascular events: A systematic review and meta-analysis. Eur J Prev Cardiol, 2016. 23(9): p. 956-66.
5. Hsueh, Y.W., et al., Association of metabolically healthy obesity and elevated risk of coronary artery calcification: a systematic review and meta-analysis. PeerJ, 2020. 8: p. e8815.
6. Lin, C.J., et al., The association between metabolically healthy obesity and risk of cancer: A systematic review and meta-analysis of prospective cohort studies. Obes Rev, 2020. 21(10): p. e13049.
7. Cruz, L.C.D., et al., Low-Intensity Resistance Exercise Reduces Hyperglycemia and Enhances Glucose Control Over a 24-Hour Period in Women With Type 2 Diabetes. J Strength Cond Res, 2019. 33(10): p. 2826-2835.
8. Dempsey, P.C., et al., Interrupting prolonged sitting in type 2 diabetes: nocturnal persistence of improved glycaemic control. Diabetologia, 2017. 60(3): p. 499-507.
9. Kanamori, K., et al., Postprandial Glucose Surges after Extremely Low Carbohydrate Diet in Healthy Adults. Tohoku J Exp Med, 2017. 243(1): p. 35-39.
10. Hyde, P.N., et al., Dietary carbohydrate restriction improves metabolic syndrome independent of weight loss. JCI Insight, 2019. 4(12).
11. Schleh, M.W., et al., Energy Deficit Required for Exercise-induced Improvements in Glycemia the Next Day. Med Sci Sports Exerc, 2020. 52(4): p. 976-982.
12. Zhou, Z., et al., Are people with metabolically healthy obesity really healthy? A prospective cohort study of 381,363 UK Biobank participants. Diabetologia, 2021.
13. Araujo, J., J. Cai, and J. Stevens, Prevalence of Optimal Metabolic Health in American Adults: National Health and Nutrition Examination Survey 2009-2016.Metab Syndr Relat Disord, 2019. 17(1): p. 46-52.
14. Maffetone, P.B. and P.B. Laursen, The Prevalence of Overfat Adults and Children in the US. Front Public Health, 2017. 5: p. 290.
15. Bray, G.A., et al., The Science of Obesity Management: An Endocrine Society Scientific Statement. Endocr Rev, 2018. 39(2): p. 79-132.
16. Taylor, R. and R.R. Holman, Normal weight individuals who develop type 2 diabetes: the personal fat threshold. Clin Sci (Lond), 2015. 128(7): p. 405-10.
17. Elías-López, D., et al., Natural course of metabolically healthy phenotype and risk of developing Cardiometabolic diseases: a three years follow-up study. BMC Endocrine Disorders, 2021. 21(1): p. 85.
18. Shakoor, H., et al., Effect of Calorie Restriction and Exercise on Type 2 Diabetes. Pril (Makedon Akad Nauk Umet Odd Med Nauki), 2021. 42(1): p. 109-126.
19. Uusitupa, M., et al., Prevention of Type 2 Diabetes by Lifestyle Changes: A Systematic Review and Meta-Analysis. Nutrients, 2019. 11(11).
20. Ross, R., et al., Reduction in obesity and related comorbid conditions after diet-induced weight loss or exercise-induced weight loss in men. A randomized, controlled trial. Ann Intern Med, 2000. 133(2): p. 92-103.
21. Ross, R., et al., Exercise-induced reduction in obesity and insulin resistance in women: a randomized controlled trial. Obes Res, 2004. 12(5): p. 789-98.
22. Vissers, D., et al., The effect of exercise on visceral adipose tissue in overweight adults: a systematic review and meta-analysis. PLoS One, 2013. 8(2): p. e56415.





Related Content
Are Oral Testosterone Replacement Formulations Legit?
Jun 15, 2025
At What Point Does Visceral Fat Accumulation Start?
Apr 23, 2025
How Do You Game A DEXA?
Apr 02, 2025